NOT JUST LYME DISEASE: WHAT YOU SHOULD KNOW ABOUT NEW TICK SPECIES AND THE DISEASES THEY CARRY
Viruses, bacteria, bugs, oh my…. pathogens that wreak havoc on our lives seems to be the topic on everyone’s mind these days. While we’re so busy dealing with COVID, it’s easy to forget about a major silent pandemic – tick-borne illnesses – that are having an increasing impact on our health.
Lyme disease, the most recognized and common tick-related infection caused by the Borrelia burgdorferi bacteria, is acknowledged in the mainstream health conversation as a pervasive threat with nearly 30,000 reported cases annually and an incidence higher than breast cancer (5). Unfortunately, new findings indicated that not only do we have to worry about Lyme, we have to consider the other multiple co-infections can be transmitted alone or in addition to borrelia, which are also on the rise. Especially as people spend more time outdoors amidst months of quarantine, Lyme and various tick-related diseases have increased as well, also complicating coronavirus pandemic detection issues in some areas such as NY state and Michigan (5).
Is it COVID…or Lyme?
Lyme disease is a multisystem illness referred to as “the great imitator”, many times with a classic bullseye rash, flu-like symptoms, and myriad symptoms replicating conditions associated with numerous other diseases and health-impaired states, ranging from cardiac to neurological to rheumatic illnesses (5). As if we don’t have enough to worry about with COVID, more less-known tick-associated diseases are not only confusing proper diagnoses related to vector-borne illnesses, they are actually mimicking COVID symptoms in many areas. Residents in various parts of the country (such as Michigan) are seeing a growing number of anaplasmosis infection cases increase, with flu-like symptoms that easily cause COVID concern.
According to the CDC (3), anaplasmosis, caused by the bacterium Anaplasma phagocytophilum and transmitted from the black-legged and the western black-legged tick, is one of the main Lyme and COVID mimickers. Symptoms are typically seen 1-5 days after being bit and can include typical symptoms such as(1).
- Skin rash
- Fatigue
- Fever, chills
- Severe headache
- Muscle aches
- Nausea, vomiting, diarrhea, loss of appetite
Early detection and prompt treatment are necessary to avoid severe illness that can lead to long-term debilitating damage to joints, the heart, and the nervous system, as well as death.
Like with COVID (or any other illness), having underlying health conditions, an already-compromised immune system, and being older can all increase the risk of illness severity (3).
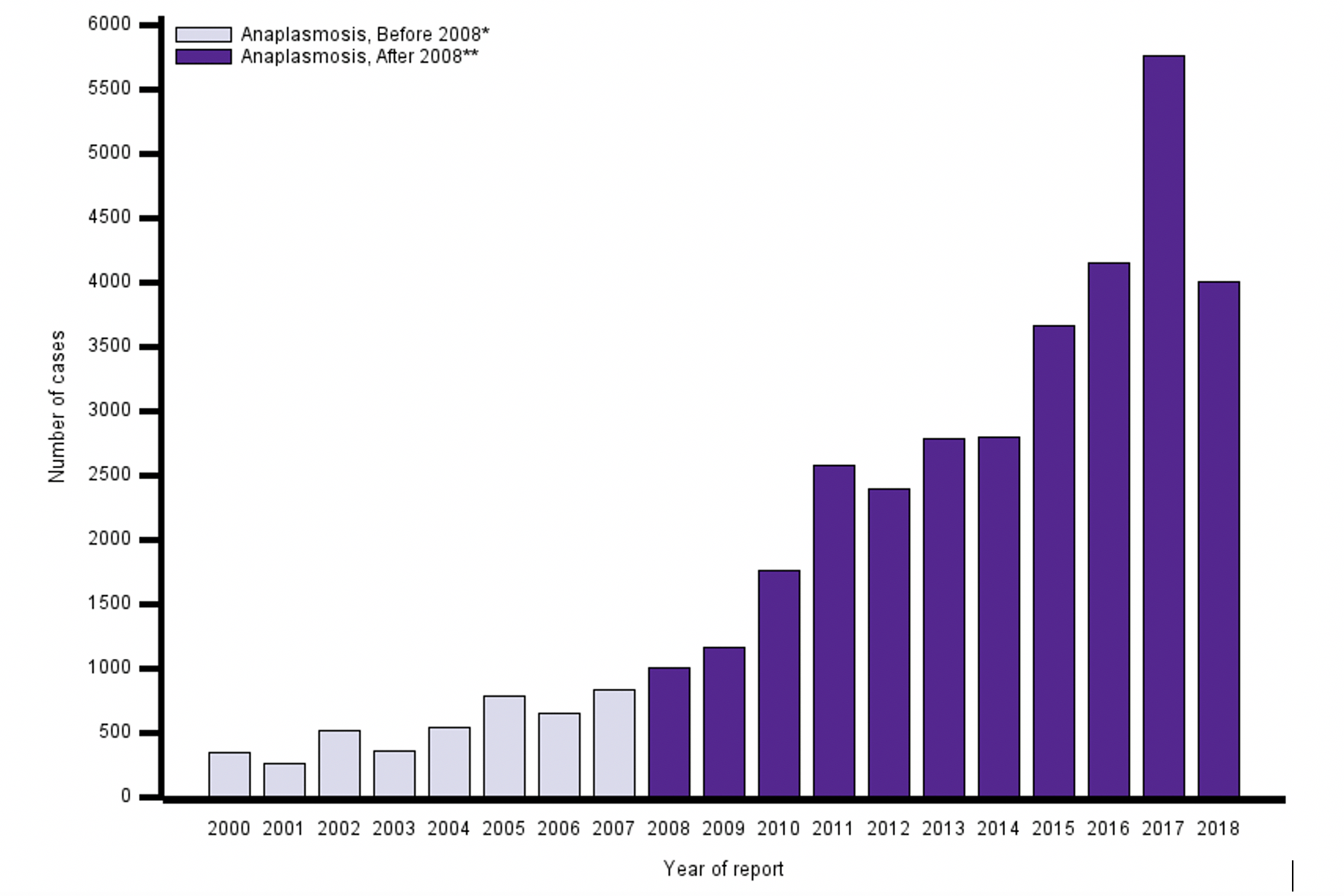
Anaplasmosis cases have been slowly rising since the year 2000, with peak months in the summer and later fall, including October and November. Geographically, the northeast and upper midwestern regions of the US suffer from the most anaplasmosis cases, but it has also been documented in newer regions such as Michigan, New York, and Virginia, and throughout the country where the black-legged tick has spread (3).
Additionally, the other various ticks and insects that carry the Borrelia bacteria causing Lyme Disease and co-infections are important to be aware of as we look for ways to protect ourselves and our families from biological threats.
Not Just Lyme Disease: Other Diseases Spread By Ticks
There has been a 3-fold increase in insect-related disease in the United State, and while Lyme and anaplasmosis are the most common tick-borne illnesses, other serious tick-related infections caused by ticks that deserve attention. Like Lyme, these other ticks and the diseases they can carry will begin to spread to other regions across the US. According to the CDC, we are only treating one out of every ten cases of Lyme disease itself – never mind the other tick-borne infections-- so awareness is key (6).
The following information provided by the CDC shows some of the primary tick-related diseases in the US (4):
- Anaplasmosis is transmitted to humans by tick bites primarily from the black-legged tick (Ixodes scapularis) in the northeastern and upper midwestern U.S. and the western black-legged tick (Ixodes pacificus) along the Pacific coast.
- Babesiosis is caused by microscopic parasites that infect red blood cells. Most human cases of babesiosis in the U.S. are caused by Babesia microti. Babesia microti is transmitted by the black-legged tick (Ixodes scapularis) and is found primarily in the northeast and upper midwest.
- Borrelia mayonii infection has recently been described as a cause of illness in the upper midwestern United States. It has been found in black-legged ticks (Ixodes scapularis) in Minnesota and Wisconsin. Borrelia mayonii is a new species and is the only species besides B. burgdorferi known to cause Lyme disease in North America.
- Borrelia miyamotoi infection has recently been described as a cause of illness in the U.S. It is transmitted by the black-legged tick (Ixodes scapularis) and has a range similar to that of Lyme disease.
- Bourbon virus infection has been identified in a limited number of patients in the Midwest and the southern United States. At this time, we do not know if the virus might be found in other areas of the United States.
- Colorado tick fever is caused by a virus transmitted by the Rocky Mountain wood tick (Dermacentor andersoni). It occurs in the Rocky Mountain states at elevations of 4,000 to 10,500 feet.
- Ehrlichiosis is transmitted to humans by the lone star tick (Ambylomma americanum), found primarily in the southcentral and eastern U.S.
- Heartland virus cases have been identified in the Midwestern and southern United States. Studies suggest that Lone Star ticks can transmit the virus. It is unknown if the virus may be found in other areas of the U.S.
- Lyme disease is transmitted by the black-legged tick (Ixodes scapularis) in the northeastern U.S. and upper midwestern U.S. and the western black-legged tick (Ixodes pacificus) along the Pacific coast.
- Powassan disease is transmitted by the black-legged tick (Ixodes scapularis) and the groundhog tick (Ixodes cookei). Cases have been reported primarily from northeastern states and the Great Lakes region.
- Rickettsia parkeri rickettsiosis rickettsiosis is transmitted to humans by the Gulf Coast tick (Amblyomma maculatum).
- Rocky Mountain spotted fever (RMSF) is transmitted by the American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni), and the brown dog tick (Rhipicephalus sangunineus) in the U.S. The brown dog tick and other tick species are associated with RMSF in Central and South America.
- STARI (Southern tick-associated rash illness) is transmitted via bites from the lone star tick (Ambylomma americanum), found in the southeastern and eastern U.S.
- Tickborne relapsing fever (TBRF) is transmitted to humans through the bite of infected soft ticks. TBRF has been reported in 15 states: Arizona, California, Colorado, Idaho, Kansas, Montana, Nevada, New Mexico, Ohio, Oklahoma, Oregon, Texas, Utah, Washington, and Wyoming and is associated with sleeping in rustic cabins and vacation homes.
- Tularemia is transmitted to humans by the dog tick (Dermacentor variabilis), the wood tick (Dermacentor andersoni), and the lone star tick (Amblyomma americanum). Tularemia occurs throughout the U.S.
- 364D rickettsiosis (Rickettsia phillipi, proposed) is transmitted to humans by the Pacific Coast tick (Dermacentor occidentalis ticks). This is a new disease that has been found in California.
According to current literature, there are other tick-borne diseases that we should be aware of, including (6):
- Cat Scratch Fever (Bartonella hensaelae)
- Rocky Mt Spotted Fever (Rickettsia rickettsii)
- Spotted fever rickettsiosis (Rickettsia parkeri)
- Human Monocytic Ehrlichiosis (Ehrilchia chaffeensis)
- Human Ewingii Ehrlichiosis (Ehrlichia ewingii)
- Q Fever (Coxiella burnetii)
- Powassan encephalitis (Flavivirus)
Is it COVID or a Tick-Borne Illness, and What Do I Do About it?
Determining if symptoms are possibly caused by COVID or stem from a tick-borne illness can be done initially by screening for symptoms specific to COVID. While the two illnesses share symptoms such as skin rash, headache, fatigue, fever, and, in some instances, long-term debilitating damage to joints, the heart, and the nervous system, COVID-specific symptoms such as loss of taste and smell can help to distinguish it from a tick-borne disease (1).
Although it can take weeks to form antibodies after getting bitten by an infected tick, individuals with a known bite and who also suffer from symptoms should seek immediate antibiotic treatment. While lab testing for Lyme Disease can sometimes be controversial and unreliable, it is typically recommended that patients undergo a course of antibiotics such as doxycycline while they wait for testing results. For diagnosing other infections like anaplasmosis, a simple blood test can determine antibodies against the pathogens while patients begin their antibiotic treatment.
Get Proactive: Preventing All Tick-Borne Illnesses
While not all ticks cause disease, and not all bites will make you sick, tick-borne illnesses are becoming more common. Because of this, it has become more important to learn ways to prevent bites, how to remove a tick if you do get bit, and what to do if you think you might have contracted a tick-borne disease.
Time in nature is essential to our health, but when we are faced with the threat of infectious pathogens from bugs and insects outdoors, we need to be mindful of the risks and take precautions to protect ourselves and our families. There are simple measures people can take to stay safe and prevent a tick bite – and the numerous tick-borne infections -- in the first place. Refer to detailed information on how to avoid tick bites as outlined by Lyme Literate Doctor and Expert Myriah Hinchey, ND, and stick to the recommended basics listed below:
- Avoid areas outdoors: In tick-infested areas, your best protection is to avoid contact with soil, leaf litter, and vegetation. However, if you garden, hike, camp, hunt, work, or otherwise spend time in the outdoors, you can still protect yourself. Avoiding the most heavily populated tick habitats such as overgrown weeds, edges of trails, stone walls, tall grass, and bushy, heavily wooded areas (1).
- Tick repellent: Using an Environmental Protection Agency-registered tick repellent that has been tested for safety and effectiveness is the second line of defense (1). If you use insect repellents, follow label directions, and apply repellent carefully. Tick and Insect Repellent: Deciding on Their Use
- Repel with protective clothing: Other preventative methods include securing your clothing and not exposing skin, wearing closed shoes, keeping long hair secured, wearing light-colored clothing. Dress to Repel!
- Frequent checks: doing routine inspections during and after being outdoors. Showering promptly, check yourself, children, and pets thoroughly for ticks, and properly removing any embedded ticks will all help to eliminate the threat of contracting a tick-borne disease (1).
- Removing a tick properly: as soon as you find a tick, removing it will reduce the likelihood of contracting any pathogens a tick may be carrying. There is a much better chance of avoiding acute and chronic Lyme and other tick-borne diseases if the tick is removed properly, if the pathogenic status of the tick is determined through testing, and if preventative measures are taken and symptoms are identified effectively within a critical time period after getting bit. This approach can help to prevent an active infection and determine a treatment protocol if necessary.
Now What? Tick-Borne Illness Treatment Protocols:
Treatment protocols, should you get bit and show signs of an active infection, include a recommended course of antibiotic therapy as well as adjunctive herbal remedies that are evidence-based and clinically proven to be effective.
Acute Lyme Disease Treatment:
Dr. Myriah Hinchey recommends treating acute Lyme and co-infections from a confirmed infected tick with the appropriate antibiotics (typically 21 days of doxycycline ) within a four-day window of the bite for the best results.*
Natural Herbal Medicine Treatment Support:
When done appropriately, findings indicate that introducing herbs early on with the antibiotics or even before the antibiotics are prescribed, resulting in very few patients transitioning to chronic Lyme Disease, which is far more difficult to treat.
Using high-quality products and manufacturers who follow the FDA Good Manufacturing Practices (GMP) and are FDA cGMP Compliant is essential to guarantee potency, safety, purity, and effectiveness of herbal products.
In conclusion, prevention is always the best medicine for any threat to our health. Making sure we are living balanced lives that support immune health is foundationally essential to our ability to deal with infectious threats that should be we exposed. When all else fails, being prepared with proper diagnostic tools and an integrative treatment plan that targets the root cause of health imbalances will be our best defense against disease and support long-term health and recovery.
*This article is for educational purposes only. It is not, nor is it intended to be, a substitute for professional medical advice, diagnosis, or treatment and should never be relied upon for specific medical advice.
References:
(1) - Stitt, C. (n.d.). Tick disease with coronavirus-like symptoms is on a rise in Michigan. Detroit Free Press. Retrieved September 16, 2020, from https://www.freep.com/story/news/local/michigan/2020/07/06/tick-disease-and-coronavirus-difficult-distinguish-year/5318549002/
(2) - Lyme Disease and Other Diseases Carried by Ticks. (n.d.). Retrieved September 16, 2020, from https://www.health.ny.gov/diseases/communicable/lyme/
(3) - (2019, January 11). Anaplasmosis home | CDC. Centers for Disease Control and Prevention. https://www.cdc.gov/anaplasmosis/index.html
(4) - (2020, April 2). Tickborne diseases of the United States | CDC. Centers for Disease Control and Prevention. https://www.cdc.gov/ticks/diseases/index.html
(5) - Tick-borne disease with symptoms similar to COVID-19 on the rise in New York state. (2020, June 12). [Text.Articlehttps://www.fox6now.com/news/tick-borne-disease-with-symptoms-similar-to-covid-19-on-the-rise-in-new-york-state">https://www.fox6now.com/news/tick-borne-disease-with-symptoms-similar-to-covid-19-on-the-rise-in-new-york-state
(6) - https://www.une.edu/sites/default/files/tickborne_diseases_hubbell_2020.pdf